Abstract
Primary refractory and relapsed acute myeloid leukemia (PR-AML) are associated with a very dismal prognosis. Allogeneic stem cell transplantation (allo-HSCT) is the only salvage option with curative potential in this situation. Since the disease status at transplant remains one of the main prognostic factors it is critical to reach complete remission (CR) at this stage. Gemtuzumab ozogamicin (GO) is a humanized anti-CD33 antibody conjugated with the cytotoxic antitumor antibiotic calicheamicin, whose results in salvage therapy remain debated. Here, we tested the combination of fractionated GO (fGO, 3mg/m² day 1, 3 and 7) with intensive chemotherapy, mainly consisting in cytarabine (1g/m² twice daily in day 1-5) and mitoxantrone (12mg/m² day 1, 2 and 3) (MYLODAM protocol).
The present single center retrospective analysis aimed to assess the outcomes of PR-AML patients treated by GO associated with intensive chemotherapy. The following prognostic factors were recorded: age, cytogenetics, molecular data, blood cell counts, organ failure, and duration of first complete remission. The primary endpoints of this study were the efficacy and safety profile of this salvage strategy. We also attempted to define predictive factors to survival and response after salvage. The ELN 2017 classification was used for prognostic assessment and definition of response.
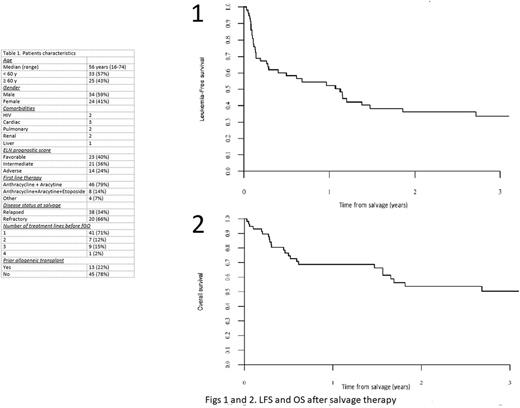
Fifty-eight patients were included. Patients' characteristics are shown in Table 1. Median age at salvage was 56 (range 16-74) years. Thirty-six (62%) received MYLODAM and 14 (24%) had fGO combined with cytarabine (1g/m² twice daily in day 1-5) and daunorubicine (60mg/m² day 1,2 and 3). Forty-six patients (79%) were monitored by molecular biology for minimal residual disease (MRD). The overall response rate was 67% (17% CRi, 17% CR and 33% CRMRD-). Median leukemia-free survival (LFS) and overall survival (OS) were 13.5 months (95% CI: 6-21) and 50 months (95% CI: 11-90) respectively (Figs 1 and 2). LFS and OS at 2 years were 36% (95%CI: 23 - 49) and 54% (95%CI: 39 - 68), respectively. Therapy-related mortality was observed in 7% (n=4) of the patients caused by 2 sepsis and 1 hemorrhagic syndrome. Three patients developed a sinusoidal obstruction syndrome (SOS), 2 of moderate and 1 of severe grade leading to death. In multivariate analysis, LFS was associated with FLT3 mutations (HR=0.33, 95%CI: 0.11-0.97) and adverse ELN risk group (HR=3.5, 95% CI: 1.5-8.2).
On the whole, 28 (48%) patients could proceed to allo-HSCT. For this subgroup, LFS and OS at 2 years were 57 % (95% CI: 36 - 77) and 69 % (95% CI: 49 - 89), respectively. The cumulative incidences of grade II-IV acute GVHD and chronic GVHD were 40% and 45.5%, respectively. At 2 years, non-relapse mortality was 16 % (95% CI: 8.5 - 33.3). Despite policy of our center to prevent SOS in this high risk patients by using Defibrotide prophylaxis, 5 SOS syndromes occurred during allogenic transplant with 3 moderate and 2 very severe forms, with no SOS related-deaths.
In summary, we conclude that, in a "real-life" setting, fGO associated with intensive chemotherapy (mainly MYLODAM) can be an effective and safe salvage regimen in patients with PR-AML, allowing in two-thirds of the cases a response achievement, and in half of the patients a bridge to allo-HSCT with encouraging outcomes.
Mohty: Sanofi: Honoraria, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal